THERAGNOSTICS- Lu-177-PSMA treatment for metastatic prostate cancer – case examples
 Prostate specific membrane antigen (PSMA) is a membrane glycoprotein with enzymatic activity (as explained in vol.1 no.2. by Jean-Luc Urbain). It is highly expressed in high-risk prostate cancer and therefore PSMA could be a basis for theragnostics. 177Lu-PSMA radioligand therapy is mainly used for patients with end-stage prostate cancer, but it can be used earlier. I describe here three patients: one patient with a multiple recurrences and one with extensive metastastic disease during the first visit, and one patient where it was used as first-line treatment. All these patients demonstrated a major response with 177Lu-PSMA radioligand therapy, i.e. complete response by imaging and substantial reduction of PSA. 177Lu-PSMA radioligand therapy gave only mild adverse effects.
Prostate specific membrane antigen (PSMA) is a membrane glycoprotein with enzymatic activity (as explained in vol.1 no.2. by Jean-Luc Urbain). It is highly expressed in high-risk prostate cancer and therefore PSMA could be a basis for theragnostics. 177Lu-PSMA radioligand therapy is mainly used for patients with end-stage prostate cancer, but it can be used earlier. I describe here three patients: one patient with a multiple recurrences and one with extensive metastastic disease during the first visit, and one patient where it was used as first-line treatment. All these patients demonstrated a major response with 177Lu-PSMA radioligand therapy, i.e. complete response by imaging and substantial reduction of PSA. 177Lu-PSMA radioligand therapy gave only mild adverse effects.
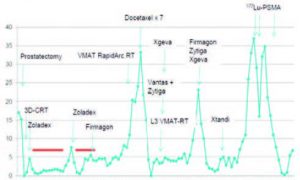
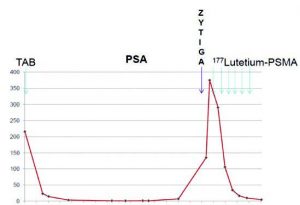
Our first patient had hypertension and diabetes for years. Primarily PSA increased from 4.6 to 17 ng/ml within 6 months. Diagnosis was done based on second round of biopsies 16 years ago when GS 6 (3+3) prostate adenocarcinoma was found in both lobes. Hormonal therapy was started with leuprorelin and bicalutamide. Prostatectomy was performed 6 months later. Tumor was very large and it was infiltrating also to seminal vesicles, consistent with staging pT3b. The full case history including serum PSA behavior is shown schematically in Fig.1, but briefly the case history is as follows.
One year later he got external beam radiation therapy to prostate fossa up to 70 Gy, bicalutamide and casodex were used for 3 years, until goserelin was started for 2 years. Bicalutamide was re-started one year later due to PSA increase (up to 4.1 ng/ml). Degarelix was introduced 2 years later for one year. Simultaneously, choline-PET-positive para-iliac and paracaval lymph nodes were irradiated up to 70/2 Gy. However, in PSA continued to increase up to 24 ng/ml and 7 cycles of docetaxel were given with partial response. Four months later, skeletal metastases were found in MRI, and palliative radiotherapy to lumbosarcal region was given. Histrelin acetate device was implanted for castration. Abiraterone and denosumab were started, but they were stopped due to the pain in muscles and joints in four months. The castration implant removed and abiraterone started again for 4 months. Denosumab was also started and continued for more than a year.
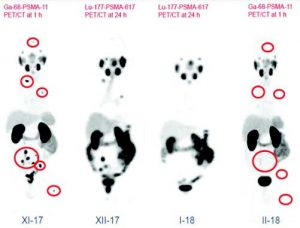
Degarelix was restarted, but it was changed to leuprorelin due to local and systemic reaction. He also got radiation therapy to choline positive upper retroperitoneal and mediastinal lymph nodes. Enzalutamide was also started but it had to be stopped in one month due to epileptic seizure. Six month later, dexamethasone combined with cyclophosphamide started to improve immunogenic response, but it had to be stopped due to the diarrhea, swelling and infection. Abiraterone started again, but four months later PSA was 33 ng/ml. On the same day in Ga-68-PSMA-PET-CT at demonstrated active uptakes in very small lymph nodes on the left side of obturator region, in upper level in para-aortal and in para-caval lymph nodes and in retrocrural region, in the middle of left mediastinum and in supraclavicular region as well. The total volume of the disease estimated to be 20 cm3.
177Lu-PSMA-617 treatments were given in July, August and October 2016 using 6 week intervals. PSA nadir 0.0 ng/ml was achieved on in March 2017. Complete response was seen in 68Ga-PSMA-11 PET-CT in March 2017 (Fig. 1, lower panel right). The patient is still alive and followed without any specific cancer therapy until January 2018. However, he felt down and broke his femur which was operated. The man is now 82 years.
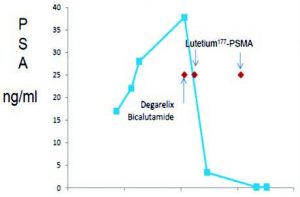
The second patient described here had primarily nocturia, pollacisuria and weak urinary flow resulting in more specific clinical studies four years ago. Initial S-PSA was 216 ng/ml. The biopsies revealed a Gleason Score (GS) 9 (5+4) adenocarcinoma with perineural invasion and extracapsular growth. Clinically the patient was T4, but there were no skeletal metastases in bone scintigraphy. Total androgen blockade (TAB) with leuprorelin plus bicalutamide was started for locally advanced prostate cancer with bilateral hydronephrosis and serum creatinine value 150. After bilateral pyelostomy operations, the patient could also urinate normally twice a day. TAB continued until March 2017. Bone scintigraphy already demostrated a superscan, and CT showed bone metastases with serum PSA value 135 ng/ml, without visceral metastases. At the end of March bicalutamide was stopped and abiraterone was started. Abiraterone was again stopped when 177Lutetium-PSMA started. Patient refused to take any chemotherapy.
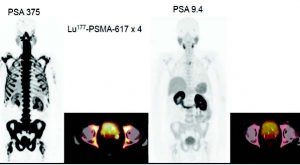
Ga-68-PSMA-PET/CT was performed in April 2017. It revealed an active and aggressive prostate malignancy in the left seminal vesicle region and extensive wide-spread strongly PSMA-positive skeletal disease. The Soloway classification was 3+/3, because extremely high uptakes in lower thoracic spine and sacrum and signs of bone marrow expansion existed. The SUVmax-values were higher than 27, while values higher than 3 are considered pathologic. The serum PSA value was 375 ng/ml.
177Lu-PSMA therapy started in May 2017. It caused tiredness and he had also swelling in foots and ankles, but surgical stockings helped that. The patient had also severe depression and anguish. Following 4th treatment in September 2017 man had nausea and emesis. After 6th treatment he had no nausea and general feeling was also good. This man is now 70 years old.
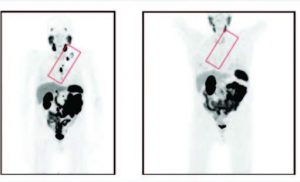
An interim control Ga-68-PSMA-11-PET/CT was performed at Docrates Cancer Center in late October 2017. The serum value was then 9.4 ng/ml. Fig. 2 demonstrates the Ga-68-PSMA-11-PET/CT.studies performed in late April and late October 2017, i.e. before therapies and 4 weeks after the 4th cycle. In the base line study an extensive skeletal disease can be seen in the MIP-image and also in pelvic fusion image (PET on CT). Normal organs, i.e. salivary and lacrimal glands, liver, spleen hardly visualize in the MIP-image. Additionally, an uptake is seen in the large prostate and in the left seminal vesicle. The interim control PET MIP-image reveals normal organs such as salivary and lacrimal glands, liver, spleen, kidneys and urinary bladder. Very little activity can be observed in the thoracic vertebra (Th 3). In interim control pelvic fusion image (PET on CT) there is no activity in the large prostate nor in the left seminal vesicle.
In control Ga-68-PSMA-PET/CT on in mid-January 2018 at Docrates Cancer Center and 6 weeks after the 6th cycle the active and aggressive prostate malignancy in the left seminal vesicle region had totally disappeared. Similarly, an extensive wide.spread strongly PSMA-positive skeletal disease, original classification probably 3+/3, had responded in all regions. There was only one subtle uptake on the left in Th3 which could be seen as in Fig.2, but the activity could already be considered normal, because the SUVmax value was only 3.8. This was considered as a dramatic response. PSA decreased from 375 ng/ml down to 4.2 ng/ml during the follow-up 177Lu-PSMA therapy. This is shown in Fig. 2.
Case 3. Aggressive GS 9 /4+5) prostate cancer in biopsies was found with PSA 28. Man was 59 years. Based on staging 4 by CT and bone scan, man was told that the given therapies according to National and International guidelines are not curative. Therefore he looked second opinion from DCC. Endorectal multiparametric prostate MRI together with NaF- and 68Ga-PSMA-PET-CT confirmed the staging to be T4N1M1. A 9×23 mm lymph node chain and a separate 7 mm node in the mesorectum on the left side, a 3 and a 5 mm suspicious node on the right side, and more cranially in the mesorectum at least two 7 mm nodes, a 9 mm obturator and a 9 mm external iliac node on the left and a 7 mm external iliac node, on the right M1a: 10 mm right common iliac node. In 68Ga-PSMA-PET-CT active and aggressive prostate malignancy was observed mainly in the left lobe with local extension and extensive lymph node disease in the pelvic spaces, the lymph node disease located predominantly on the left with a total volume of 75 cm3 and it was very active with SUVmax ad 47.
There was lymph node disease in obturator, perirectal, parailiac (ext/int), common iliac, presacral nodes. Wide-spread skeletal disease with low volume (25 cm3), classification 1/3, but with high uptakes e.g. in lower spine (SUVmax >30); solitary metastases in the skull, spine, thorax and left proximal femur. Since the disease was shown to be aggressive, man was young and very healthy, and the cancer cells appeared to be avid for PSMA we decided to start the therapy using Lutetium177.PSMA together with more traditional hormone treatment. Patient decided to stop smoking also.
In the first early response evaluation PSA went down 37.8 to 0.16 ng/ml and the response was confirmed also by 68Ga-PSMA-PET-CT scanning, demonstrating practically complete response by imaging. Earlier active and aggressive prostate malignancy was not anymore active (SUVmax < 2.7). The local extension and extensive and active lymph node disease in the pelvic and retroperitoneal spaces (obturator, perirectal, parailiac (ext/int), common iliac, presacral nodes) had completely vanished. Similarly, the wide.spread skeletal disease (skull, spine, thorax and left proximal femur) had fully disappeared. The PSMA-positive disease (skeletal 25 cm3 + lymph nodes 75 cm3) demonstrated a visual metabolic complete response. Quantitative « PERCIST »-response turned out to be -93%.