Brain imaging in nuclear medicine
When visiting a patient with atypical cognitive defects or movement disorder, refractory epilepsy or, during follow-up of a brain neoplasm, brain imaging studies in nuclear medicine might help you to accurately evaluate your patient’s disorder.
Cerebral blood flow studies with Ceretec® or Neurolite®, as well as brain metabolism studies with 18FDG (fluorodeoxyglucose) (table 1) can help determine the cause of dementia (Alzheimer’s disease (AD), fronto-temporal dementia (FTD) or dementia with Lewy body disease (DLBD)) and/or a movement disorder unresponsive to medications (multiple system atrophy, corticobasal degeneration or supranuclear palsy). In addition, these same exams can also help localize an epileptic focus in case of refractory epilepsy. Furthermore, the degree of glucose hypermetabolism with 18FDG helps determine the aggressiveness of a tumor and, later on, to evaluate the responsiveness to treatment and to look for recurrence when conventional imaging cannot distinguish post-irradiation changes from recurrence.
The brain nuclear imaging possibilities are multiple, and this is without taking into account the possibilities of more specific tracers that could eventually reach clinical availability, such as dopaminergic tracer (Datscan®), tumoral tracer (18FET) or amyloid tracer used in dementia diagnosis.
The most frequent and recognized use remains dementia imaging, which will be the subject of this article.
Alzheimer’s disease
According to the most recent statistics, approximately 500,000 Canadians suffer either from AD or a similar dementia. By 2038, this number will double. Currently, the medications available to decrease or slow down the progression of cognitive symptoms are useful only in AD, justifying the need to obtain a precise diagnosis whenever possible before giving such medications, which cost is not negligible. Furthermore, having the right diagnosis is helpful when discussing with families about the disease and prognosis.
SPECT vs PET? What is the difference?
Depending on different hospitals, two types of brain nuclear imaging are available. SPECT (Single Photon Emission Computed Tomography) is a tomographic test (3 D slices) available in all nuclear medicine departments since it’s done with conventional gamma cameras. It uses a blood flow tracer with technetium-99m to image brain perfusion.
Brain FDG PET (positron emission tomography) is available in different PET centers in Quebec (table 1). It uses glucose to study brain metabolism. With regards to dementia, the bio-distribution of the two types of radiotracers is similar. PET studies are somewhat more accurate, however, when not available, SPECT is a good alternative. (Note: to simplify reading in the following paragraphs, the term hypometabolism will be used when referring to a PET exam, while the term hypoperfusion will be used when referring to SPECT).
Metabolic patterns of different types of dementia
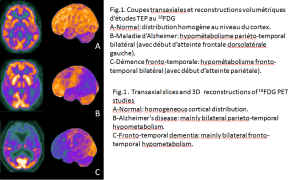
Distinguishing AD from FTD is sometimes difficult in clinical routine, especially when a frontal syndrome complicates the presentation. With nuclear brain imaging, this distinction is usually easy to make. In early AD, bilateral parieto-temporal hypometabolism (figure 1B) is seen, often asymmetrical, which will eventually progress toward dorsolateral frontal regions. There will also be an early involvement of the posterior cingulate gyrus and precuneus. By opposition, FTD will show a predominantly bilateral frontotemporal hypometabolism, most marked in their frontal aspect (figure 1C). DLBD will show defects similar to AD, with further extension to the occipital region (table 2). Vascular dementia is rather a conventional imaging diagnosis, with focal asymmetrical defects that can be seen.
Before prescribing a brain imaging study!
There are confounding factors important to know. For example, uncontrolled hypothyroidism and major depressive disorder can cause hypometabolism similar to AD. It is thus essential to establish that TSH is normal before sending your patient for a brain study. Besides, TSH detection is rarely a problem. Likewise, it is as important to wait for the resolution of a depressive episode to avoid misinterpretation of the results, necessitating the need to repeat the exam at a later date and, of course, incurring unnecessary costs and stress. This is also true for any psychiatric syndrome. It is also worth mentioning that DLBD and Parkinson’s dementia have similar metabolic patterns and therefore cannot be distinguished from one another by either PET nor SPECT.
In conclusion, when would it be best to request for these exams? Well, mainly whenever there is uncertainty between the diagnosis of AD and FTD. On the other hand, the use of SPECT or PET is not recommended when one wants to differentiate DLBD from Parkinson’s dementia, since these have the same metabolic pattern. Finally, it is imperative to wait for the resolution of a depressive or psychiatric syndrome before requesting such tests.
Table 1 :
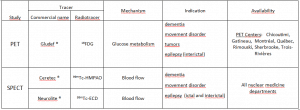
Table 2 :
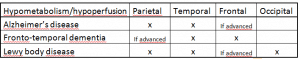
Table 3 :