Brain perfusion spect, a highly useful test for the diagnosis of the dementias
Philip F. Cohen, MD FRCP(C)
Division Head, Nuclear Medicine
Lions Gate Hospital
Associate Professor Radiology
University of British Columbia
Brain perfusion SPECT is highly useful for the diagnosis of the dementias, including Alzheimer’s disease, Frontotemporal Dementia and Lewy Body Disease. Studies of the accuracy of SPECT for diagnosing Alzheimer’s disease report sensitivities of 65%–85% and specificities (for other dementias) of 72%–87%(1). In the largest study to date, both HMPAO SPECT and 18F-FDG PET were able to completely separate 26 AD cases from controls(2). SPECT has been advocated over 18F-FDG PET on the basis of its wider availability, lower cost and perceived better patient tolerability, although a recent review suggested 18F-FDG PET had greater diagnostic accuracy over Brain Perfusion SPECT, where available(3). Guidelines of the European Association of Nuclear Medicine and the American College of Radiology endorse the clinical use of Brain Perfusion SPECT in the workup and diagnosis of dementia(4,5).
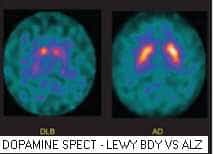
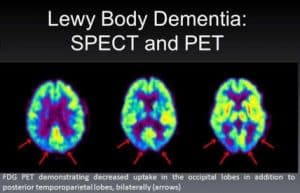
Brain perfusion SPECT is useful because the clinical diagnosis of dementia is often inaccurate, especially in early dementia when patients have only mild cognitive impairment, and can be confused with depression, bipolar disorder, metabolic disorder or multiple infarct dementia, a potentially treatable cause of dementia(6). The anatomic imaging modalities –CT and MRI– often show no abnormality. Structural abnormalities in the hippocampus, which can be seen on MRI, are currently difficult to assess in routine clinical practice. New amyloid PET tracers show promise in early detection of Alzheimer’s disease, but to date are not reimbursed for routine use(7). Brain Perfusion SPECT is widely available and reimbursed, but ideally should be performed with optimal dedicated nuclear medicine SPECT systems with high spatial resolution, three dimensional reconstruction software, parametric mapping and fan beam or multi-pinhole collimators(8). New SPECT detectors using multiple pinholes show resolutions comparable to PET detectors and can simultaneously image both perfusion and Dopamine receptor agents such as I-123 beta-CIT, to more accurately diagnose dementia with Lewy-bodies(9). Originally developed for animal studies, new detectors with multiple pinholes are now available for human brain SPECT and promise sensitivities and resolutions competitive and possibly exceeding current PET scan detectors(10).
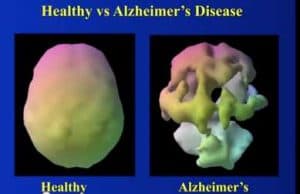
Patterns of abnormal perfusion in dementia can show very characteristic perfusion changes, although no perfusion patterns are 100% sensitive or specific. In very advanced dementias, almost completely absent cortical perfusion may be present to make all dementias essentially indistinguishable.
Scans of patients with advanced Alzheimer’s dementia usually show a typical hypo-perfusion in the tempero-parietal regions. In Frontotemporal Dementia, hypoperfusion is usually seen in the frontal cortex and frontal temporal lobes. In dementia with Lewy-Bodies, decreased perfusion is seen in the occipital cortex, and studies with SPECT dopamine tracers (DaTScan I-123 beta-CIT or Tc-99m Trodat) show decreased uptake of dopamine in the basal ganglia(9). Multi-infarct dementias show multiple perfusion defects throughout the cortex and white structures. In the earliest stages of Alzheimer’s disease, impaired memory deficit has been shown to correlate with hypometabolism of temporal mesial structures (especially the hippocampus), posterior cingulate gyrus and basal frontal cortex(11).

- Dougall NJ, Brugg KS, Ebmeier K. Systematic review of the diagnostic accuracy of 99mTc-HMPAO SPECT in Dementia, Am J Geriatr Psychiatry. 2004;12:554–570
- Herholz K, Schopphoff H, Schmidt M, et al. Direct comparison of spatially normalized PET and SPECT scans in Alzheimer’s disease. J Nucl Med. 2002;43:21–26
- O’Brien, JT, Firbank, MJ, Davison, C, Barnett, N, Bamford, C Donaldson, C Olsen, K Herholz, K Williams D 18F-FDG PET and Perfusion SPECT in the Diagnosis of Alzheimer and Lewy Body Dementias, J Nucl Med, 2014, 55: 1959-1965
- Kapucu, OL Nobili F, Varrone A, Booij J, Vander Borght T, Någren K, Darcourt J, Tatsch K, Van Laere.K EANM procedure guideline for brain perfusion SPECT using 99mTc-labelled radiopharmaceuticals, version 2 Eur J Nucl Med Mol Imaging DOI 10.1007/s00259-009-1266-y
- ACR Res. 25 – 2012, Amended 2ACR–SPR Practice Parameter for the Performance of Single Photon Emission CT (SPECT) Brain Perfusion and Brain Death Examinations014 (Res. 39)
- Woodford H.J., George J. Cognitive assessment in the elderly: a review of clinical methods DOI: http://dx.doi.org/10.1093/qjmed/hcm051 469-484 First published online: 12 June 2007
- Kubota T, Ushijima Y, Yamada K, Okuyama C, Kizu O, Nishimura T. Diagnosis of Alzheimer’s disease using brain perfusion SPECT and MR imaging: which modality achieves better diagnostic accuracy? Eur J Nucl Med Mol Imaging 2005;32:414-421.
- Juni J, Waxman A, Devous, M et al Society of Nuclear Medicine Procedure Guideline for Brain Perfusion Single Photon Emission Computed Tomography (SPECT) Using Tc-99m Radiopharmaceuticals version 2.0, approved February 7, 1999
- O’Brien JT, Colloby S, Fenwick J, et al. Dopamine transporter loss visualized with FP-CIT SPECT in the differential diagnosis of dementia with Lewy bodies. Arch Neurol. 2004;61:919–925
- Miwa K, Inubushi M, Takeuchi Y, Katafuchi T, Koizumi M, Saga T, Sasaki M Performance characteristics of a novel clustered multi-pinhole technology for simultaneous high-resolution SPECT/PET Annals of Nuclear Medicine June 2015, Volume 29, Issue 5, pp 460-466
- Bonte FJ, Harris TS, Roney CA, Hynan LS. Differential diagnosis between Alzheimer’s and frontotemporal disease by the posterior cingulate sign. J Nucl Med. 2004;45:771-4.



