Stress testing: Questions and Answers
By Raymond Russell, III, MD, PhD, FASNC, FACC
Associate Professor of Medicine
Warren Alpert Medical School of Brown University
Director, Nuclear Cardiology, Rhode Island Hospital
President, American Society of Nuclear Cardiology
Disclosures: Spouse employed by Novartis Institutes for Biomedical Research
When I recommend that a patient undergo stress testing, I try to anticipate the questions they may have about the test and how the information gained from the test will change their care. By answering these questions, I hope to help my patient make the most informed decisions concerning the stress test itself and the management decisions that arise from the stress test. Making sure that our patients are well-informed concerning their testing and treatment options is an important responsibility of any physician.
Why do I need a stress test?
Far and away, the most common reason that someone needs a stress test is because they have experienced some sort of symptom that is concerning for the presence of significant coronary artery disease (CAD), or blockages of the arteries that feed the heart. The symptom may be angina, that is, chest pressure that occurs with exertion. However, someone may have other symptoms that increase my suspicion for the presence of CAD. These may include atypical pain or pressure symptoms in someone who is at risk for CAD, or new or worsening shortness of breath with exertion.
In addition, stress testing may be performed in patients who have developed congestive heart failure and I am concerned that CAD may be causing their heart failure. Similarly, some patients who develop dangerous rhythm disturbances of the heart may undergo stress testing to help determine the cause of that rhythm. In addition, some patients may undergo stress testing because of another study, such as an echocardiogram or a coronary calcium scoring test, that was abnormal.
What is involved in a stress test?
Stress tests come in a variety of forms and every effort is made to focus the test on the patient, their capabilities with respect to exercising, and the information that is needed. The first step in the decision process is to determine what type of “stress” will be used for the study. In general, the best type of stress test is one in which the patient exercises, either on a treadmill or on a stationary bicycle. This is because there is very useful information that comes from observing how someone responds to exercise. However, physicians recognize that not all patients are able to exercise, either safely or to an adequate level, to provide diagnostic information on the stress test. For those individuals, a drug (adenosine, dipyridamole, regadenoson, or dobutamine) is given that dilates the coronary arteries that feed the heart to mimic what occurs during exercise. If a patient undergoes such a pharmacologic stress test, it is very important to follow the instructions provided to them in preparation for the stress test.
The second step in the decision process is to determine whether some type of imaging of the heart is required to increase the ability to detect decreased blood flow (ischemia) in the heart. There are several types of imaging that can be performed, nuclear perfusion imaging, echocardiographic functional imaging, or cardiac magnetic resonance perfusion imaging. In this article, I will focus on nuclear perfusion imaging. If a patient is at low risk of having CAD, and they can exercise, and they have a normal electrocardiogram, then an exercise stress test without any form of imaging is generally appropriate. If the patient has risk factors for CAD or has an established diagnosis of CAD, then imaging is likely to be an important adjunct to detect CAD. If the patient cannot exercise adequately, then they will require a pharmacologic stress test with imaging to detect CAD.
On the day of the stress test, the patient will be “prepped” for the procedure. This includes have an intravenous (i.v.) catheter inserted for the administration of a pharmacologic stress agent (if needed) and the radioactive dye to image the heart (if needed). In general, both exercise and pharmacologic stress tests are safe, but the insertion of an i.v. catheter also allows for the ability to give other medications if needed. In addition, electrocardiographic electrodes are attached to the body to record the ECG during the study.
For an exercise stress test, the patient will exercise at increasing levels of exertion up to the point that they cannot exercise any further. At this point, a radioactive dye is injected by vein and is taken up by the heart. For the pharmacologic stress test, one of the vasodilating agents is injection to increase blood flow to the heart and then the radioactive dye is injected to once again evaluate blood flow to the heart. It is not uncommon for someone to experience symptoms such as shortness of breath or chest pain during the injection of the pharmacologic agents. The patient’s blood pressure and electrocardiogram are monitored continuously during the stress test by a nurse or physician and they will ask about any symptoms that the patient may have.
After the radioactive dye is injected, the patient will rest for 10-45 minutes before being placed in a special camera that detects the radioactivity taken up by the heart. Depending on the type of camera, a patient may lay under/inside the camera for 5-30 minutes. In addition to the images obtained after stress testing, a patient may need to have resting images taken for comparison. This involves all of the steps described above, except for the stress testing.
What information comes from the stress test?
The stress test and imaging that are performed provide very valuable information for the referring physician. An example of a normal stress test, in which the blood flow is normal throughout the heart, is shown in figure 1. An example of an abnormal stress test, with significant decreases in blood flow, is shown in figure 2.
The information from the stress test, in addition to the imaging study provides a “yes/no” answer to the question of whether someone had blockages in the coronary arteries. But more importantly, the data provides an assessment of risk of having a heart attack (myocardial infarction) or experiencing cardiac death over the next year. In other words, someone who has a small decrease in blood flow to their heart on the stress test is at low risk of having a heart attack or cardiac death over the ensuing year and may be best served by starting with a treatment plan that focuses on medical therapy and risk factor management. In contrast, someone who has severe, diffuse decreases in blood flow would be considered at high risk of cardiac events and may be better served by undergoing a treatment plan that includes cardiac catheterization and revascularization to improve blood flow to the heart, either by angioplasty and stenting or by bypass surgery.
These are just some of the questions that I get asked when someone is undergoing a stress test, and every individual has different questions and concerns as they face testing. In addition, based on variety of factors, your stress test may not follow the exact course I have described above and the treatment decisions similarly may be different. Be sure that you understand what sort of testing your physician has recommended and that your questions are answered.

Figure 1. A normal stress test imaging study. The stress images are shown in the rows marked A and the rest images are shown in the rows marked B. The uptake of the radioactive dye is similar throughout the heart muscle shown in three different orientations: short axis (top), vertical long axis (middle), and horizontal long axis (bottom).
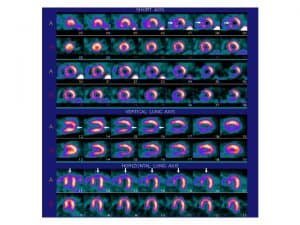
Figure 2. An abnormal stress test image. The stress and rest images are once again shown as described in Figure 1. There is decreased blood flow in the stress images, as indicated by the white arrows, that improves in the resting images. These findings are consistent with the presence of significant blockages in the coronary arteries.



